Bariatric Surgery vs. Wegovy at 12 Months: Which Delivers Lasting Results?
This is a contributed post.
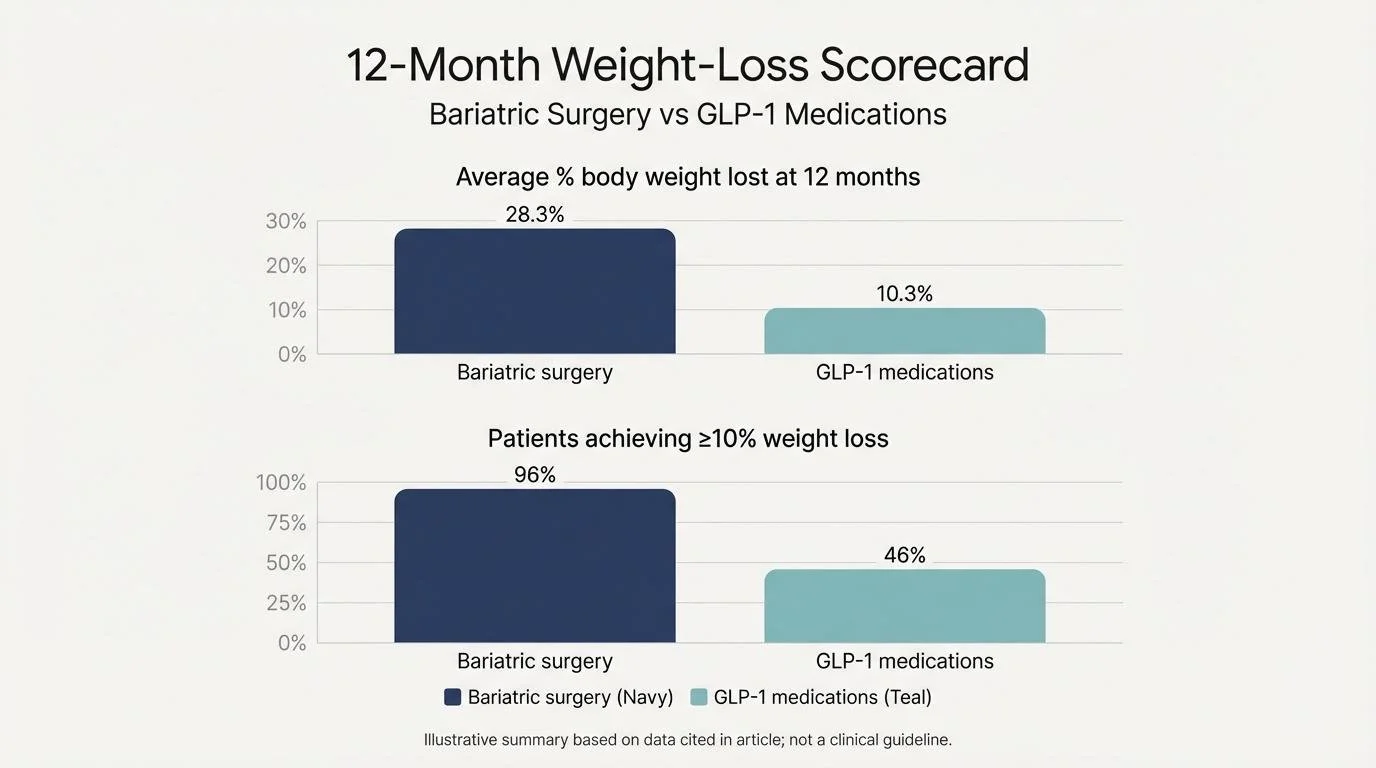
Weight-loss care now sits at a crossroads: weekly GLP-1 injections like Wegovy on one side and bariatric surgery on the other. A 2025 JAMA Surgery analysis of more than 30,000 patients showed surgery delivers about 28 percent body-weight loss at 12 months versus 10 percent on GLP-1 drugs. In the pages ahead, we’ll break down what those numbers mean for your health, wallet, and daily routine—helping you decide which path offers results that last.
1. One-year weight-loss scorecard
A midlife woman weighs the choice between metabolic surgery and weekly GLP-1 injections with care and calm.
The largest real-world comparison to date—30,458 adults in a 2025 JAMA Surgery analysis—shows surgery outpacing medication from day one. Patients who underwent gastric bypass or sleeve gastrectomy shed an average 28.3 percent of their body weight at 12 months, while those on weekly GLP-1 injections such as semaglutide (Wegovy) lost just 10.3 percent over the same period.
Put differently, surgery delivers roughly three pounds for every pound lost with medication. The edge held across age groups and insurance plans because researchers pulled weight readings from routine clinic visits, not tightly controlled trials.
Digging deeper, 96 percent of surgery patients hit at least a 10-percent drop, compared with 46 percent of GLP-1 users—a threshold many experts tie to meaningful metabolic improvement.
At 12 months, bariatric surgery delivers roughly three times more weight loss than GLP-1 medications and more patients reach at least a 10 percent drop.
If the next 12 months matter most to you, the scoreboard is clear: metabolic surgery leads the pack on early weight reduction, while GLP-1 therapy offers more modest—though nonsurgical—progress.
2. Long-term sustainability and regain
Bariatric surgery keeps most of the weight off
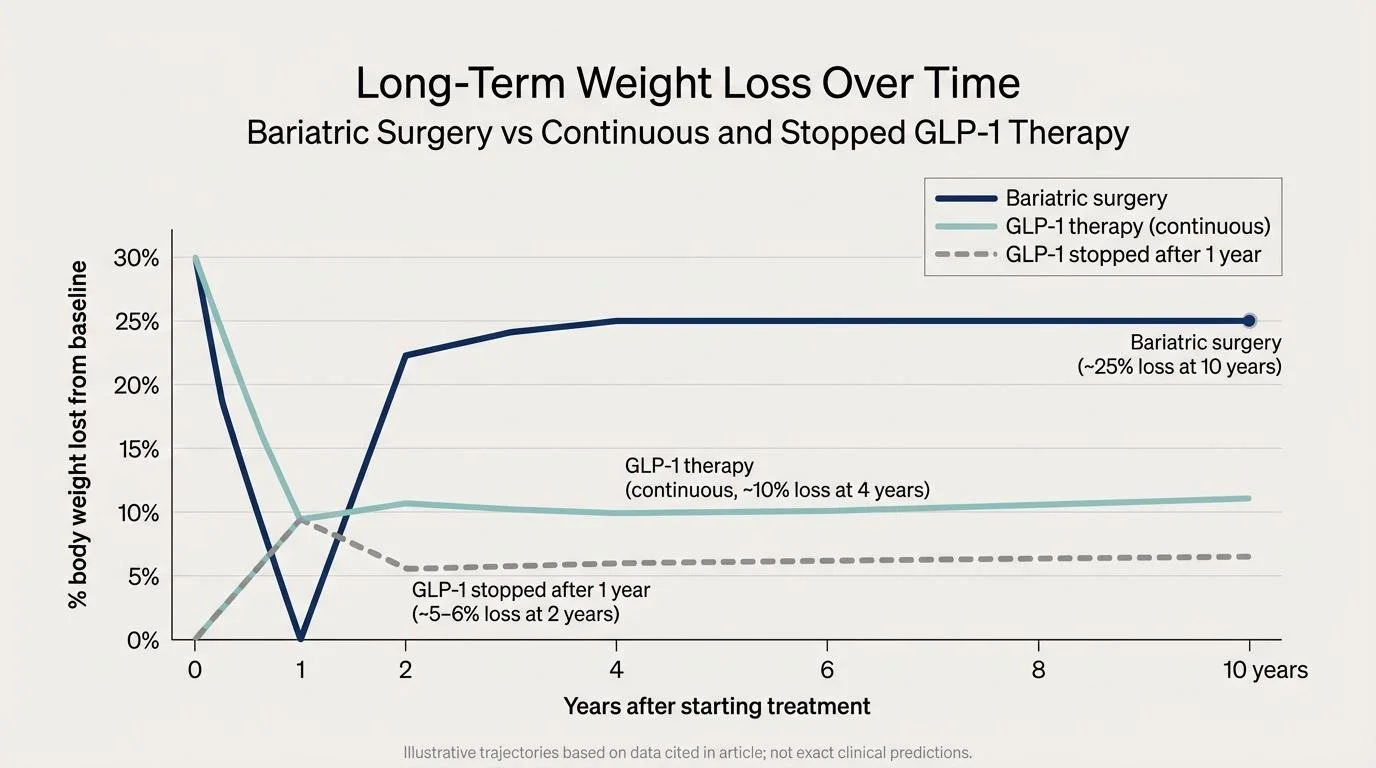
In an ASMBS meta-analysis of more than 9,000 patients, sleeve and bypass recipients maintained about 25 percent total-body weight loss at 10 years, even after a modest regain that typically begins around year two (see the 2024 PubMed-indexed study).
GLP-1 results depend on continuous use
In the STEP 1 extension, participants who stopped once-weekly semaglutide regained roughly two-thirds of their prior loss within 12 months, finishing with a net 5–6 percent drop from baseline, according to PubMed data. Ongoing therapy fares better: a 17,000-person outcomes trial reported about 10 percent weight loss remained at four years among those who stayed on Wegovy, Reuters noted.
Surgery maintains larger long-term weight loss, while GLP-1 results depend heavily on whether treatment continues or stops.
Bottom line: Surgery rewires gut anatomy and hormones, giving most patients durable weight control. GLP-1 therapy can provide meaningful, longer-term loss, yet only if you commit to ongoing treatment.
3. Health gains beyond the scale
Bariatric surgery leads the field on metabolic remission
In a 2024 review of 351 Roux-en-Y patients, 57 percent achieved complete type 2 diabetes remission at one year and 29 percent saw hypertension resolve, according to a PubMed-indexed report.
Large registries show durable benefits: gastric bypass patients cut long-term cardiovascular mortality by about 40 percent compared with matched nonsurgical peers, according to data discussed by the New England Journal of Medicine.
GLP-1 therapy improves risk factors, though less dramatically
In STEP-2, adults with obesity and diabetes taking once-weekly semaglutide saw mean A1c fall 1.6 percentage points and systolic blood pressure drop ≈7 mm Hg at 68 weeks, versus –0.4 % and –2 mm Hg with placebo, PubMed records show.
Only a minority reached medication-free diabetes remission, and most continued at least one antihypertensive.
Quality of life echoes the numbers. Surgery recipients often report ditching insulin pens, shelving the CPAP, and walking pain-free within a year. GLP-1 users describe steadier energy and smaller clothing sizes, yet less medication freedom. According to Bariatric & Metabolic Center of Colorado's overview of long-term outcomes, many post-surgery patients not only lose most of their excess weight but also see type 2 diabetes, sleep apnea, high blood pressure, fatty liver disease, and elevated lipids recede or resolve, along with better energy and mobility. That kind of multi-system payoff is what clinicians mean by a metabolic reset, while GLP-1 therapy tends to chip away at individual risk factors more gradually and only for as long as the prescription continues.
If putting diabetes or high blood pressure into the rear-view mirror is as important as trimming inches, surgery delivers the deeper, more durable health reset, while GLP-1s offer meaningful but step-wise gains that rely on continued therapy.
4. Risks and side effects: two very different journeys
Surgery: brief surgical risk, then low long-term burden
In the MBSAQIP registry of more than 200,000 cases, serious 30-day complications occurred in 2.4 percent of patients and mortality in 0.1 percent, rates similar to gallbladder removal.
The most common early issues are bleeding or infection, usually treated during the initial admission. After discharge, the main lifelong chore is a daily vitamin and mineral routine to prevent iron, B12, or calcium deficiencies. Late problems such as internal hernia or marginal ulcer appear in fewer than five percent of patients and are often fixed endoscopically or laparoscopically.
GLP-1 drugs: mild to moderate symptoms that can persist
Across pooled STEP 1–3 trials, 43.9 percent of semaglutide users reported nausea, 29.7 percent diarrhea, and 24.5 percent vomiting, roughly triple the placebo rate. These events peak during dose escalation but linger for some.
Long-term safety signals are still emerging. The FDA label lists rare pancreatitis and a possible thyroid C-cell tumor risk, and 2024 lawsuits allege severe gastroparesis in a small subset of users, according to Time magazine.
Because treatment is ongoing, side effects may return whenever the dose increases or restarts after a pause.
Large randomized trials echo those clinic numbers. SURMOUNT-4 recorded side effects in 81 percent of tirzepatide users with 7 percent discontinuing treatment, and a semaglutide study logged adverse events in 48.6 percent of participants; a concise roundup appears in this guide to weight loss drug risks.
Take-home: Surgery concentrates risk into the first few weeks, with decades of safety data showing low ongoing complication rates. GLP-1 therapy skips the operating room but carries a higher chance of persistent gastrointestinal symptoms and the possibility of yet-unknown rare events as long as the weekly pen stays in play.
5. Cost, coverage, and long-term value
Sticker price
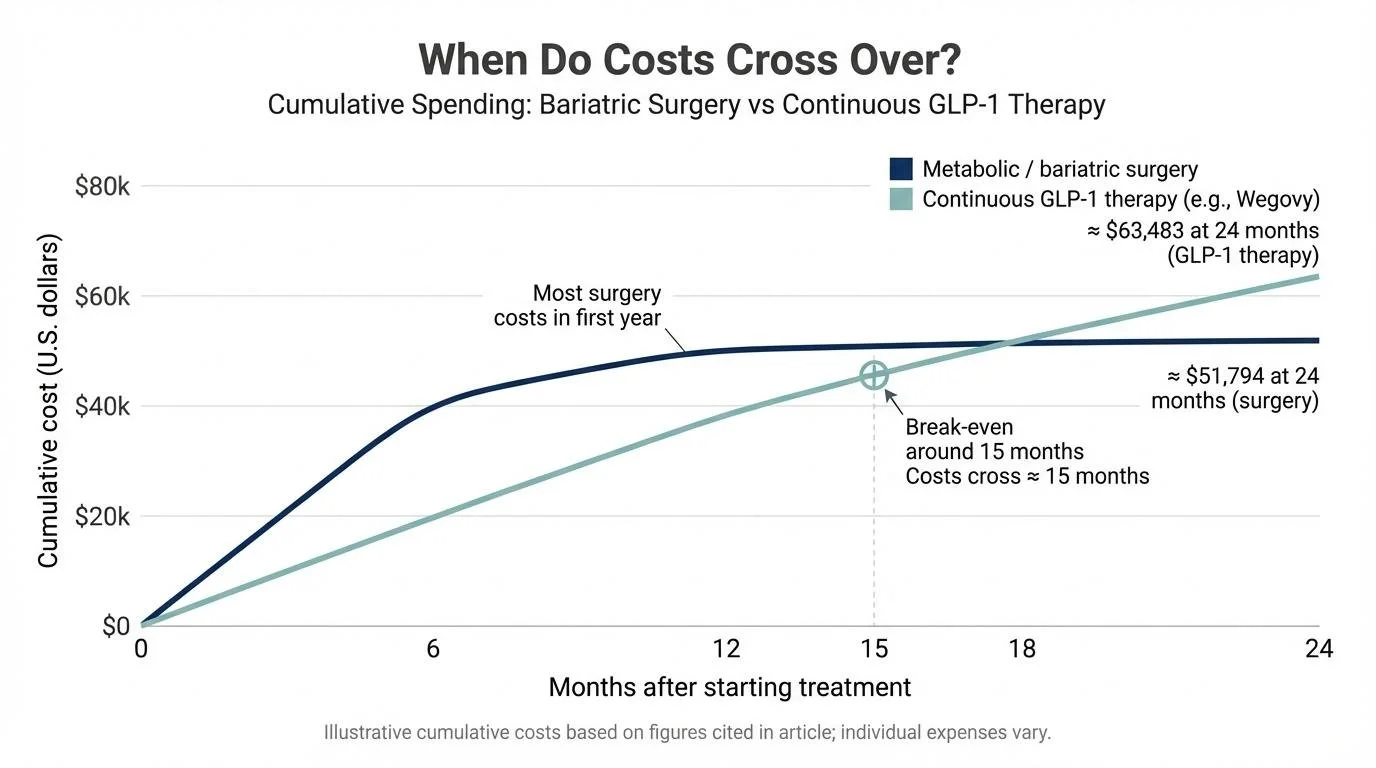
National hospital data list the average self-pay cost of a gastric sleeve at about $18,900 and gastric bypass at $23,300 before insurance or discounts.
Wegovy’s list price is $1,349 per 28-day pen, yet most uninsured patients now pay $349 per month through Novo Nordisk’s 2025 cash-pay program, while insured patients see copays that range from $0 to several hundred dollars.
Break-even math
The 2025 JAMA Surgery cohort calculated mean two-year costs of $63,483 for continuous GLP-1 therapy versus $51,794 for metabolic surgery, a difference of $11,689 in favor of surgery. Modeling from that study shows the spending curves cross at roughly 15 months.
Surgery concentrates most costs into the first year, while monthly GLP-1 prescriptions can overtake those expenses after roughly 15 months.
Insurance reality
Most commercial and Medicare Advantage plans cover bariatric surgery once BMI and comorbidity criteria are met, leaving you responsible only for the deductible and coinsurance.
Anti-obesity drugs remain patchy: about one-third of large employers cover them, and prior authorizations are common, according to KFF. Even with approval, typical copays run $25–$150 per fill.
Bottom line: Surgery concentrates spending into a single year and then falls to routine follow-up costs. GLP-1 therapy, by contrast, adds a pharmacy bill every month. At today’s prices, surgery usually becomes the cheaper option after 15 to 18 months, so the upfront sprint can win the long-distance race for many budgets.
6. Eligibility and choosing the right path
Current clinical cut-offs
Bariatric surgery: The 2022 ASMBS / IFSO statement authorizes metabolic surgery at BMI ≥ 40, or BMI ≥ 35 with at least one serious obesity-related disease. Surgery is also allowed at BMI 30–34.9 when type 2 diabetes or uncontrolled metabolic syndrome is present.
Wegovy (semaglutide 2.4 mg): FDA labeling approves use at BMI ≥ 30, or BMI 27–29.9 with a weight-related condition such as hypertension or pre-diabetes.
Medication spans a wider size range, while surgery remains the most powerful tool for severe or fast-moving disease.
When clinicians skip straight to surgery
Endocrinologists and surgeons often recommend bypass or sleeve for:
BMI ≥ 50 (super-obesity)
Insulin-dependent or worsening diabetes with looming organ damage
People who have completed six months of supervised medical therapy without success (a common insurance rule)
Blended strategies are rising
A short course of GLP-1 drugs before surgery can shrink the liver and lower anesthesia risk.
Years after surgery, the same medication may be added if weight regain exceeds about ten percent of your lowest weight, providing a reversible booster instead of a second operation.
Action step
Eligibility is only half the story. A joint consult with a bariatric surgeon and an obesity-medicine specialist will weigh your BMI, health history, insurance rules, and timing, then recommend surgery, medication, or a staged blend that fits your goals and coverage.
7. Lifestyle commitments and day-to-day reality
Life after surgery
Expect a four-stage diet (liquids → purées → soft foods → small solid meals) during the first eight weeks. Most patients feel comfortably full on ½–1 cup of food per meal.
Lifelong supplements are non-negotiable. In a two-year cohort, 60 percent maintained at least 80 percent adherence to calcium-vitamin D and B₁₂ tablets, yet lapses still produced detectable deficiencies in 15 percent of cases, PubMed data show.
Quarterly lab work and at least annual surgeon visits track nutrition and weight. Many programs also require group classes or online support sessions, vital checkpoints that help preserve habits.
Life on Wegovy
A single sub-cutaneous injection takes seconds, but treatment is chronic. Real-world data from an academic clinic show median persistence of 10.7 months; about one in three patients stop earlier because of side effects, insurance issues, or cost, according to PubMed.
Common nausea usually eases after the first few doses, yet hydration and protein targets (≈ 75 g per day) remain important to protect muscle. Skipped doses can trigger appetite rebound within days.
Follow-ups are lighter, typically every 3–6 months with an obesity-medicine provider, but each dose change may restart mild side effects.
Choosing your cadence
Surgery compresses lifestyle change into an intense first year, then depends on structured follow-up and supplements. Wegovy spreads a lighter routine of weekly injections and mindful eating over the long haul. Match the rhythm to your personality, budget, and support network, and remember: consistent habits, not bursts of willpower, move the scale in the right direction.
8. The biology behind the bite
Surgery rewires multiple gut signals at once
A sleeve or bypass removes the gastric fundus and reroutes food, leading to a 60–80 percent drop in fasting ghrelin and a post-meal rise in GLP-1 and PYY within three months, according to PubMed-indexed research. These shifts sharpen satiety, mute cravings, and may “reset” the brain’s defended weight.
Semaglutide mimics one key messenger
Wegovy provides a pharmacologic GLP-1 look-alike that binds brain receptors, cuts ad-libitum calorie intake by about 35 percent, and slows first-hour gastric emptying by roughly 27 percent, PubMed studies report. When drug levels fall, endogenous ghrelin and other appetite drivers return, so hunger control depends on steady dosing.
Translation: Surgery changes the hardware and installs new code, while semaglutide operates like a removable software patch. Many post-op patients report a lasting “food calm,” whereas medication users notice hunger control fade if they miss a dose.
9. Popularity, perception, and patient satisfaction
Wegovy ruled health headlines in 2024 after celebrities posted “weekly-pen” selfies. IQVIA data show U.S. GLP-1 prescriptions doubled between January 2023 and January 2025, while the ASMBS recorded a 24 percent drop in bariatric case volume in 2023 versus 2019 levels, according to the health analytics firm Guts & Growth.
Yet surveys tell a more layered story:
Surgery: Five-year follow-up from a Norwegian cohort found 82 percent of sleeve and duodenal-switch patients were “satisfied or very satisfied,” and 85 percent would choose surgery again, PubMed data indicate.
Wegovy: In a one-year real-world survey of 564 semaglutide users, 71 percent rated treatment “worth it,” but 28 percent cited cost or gastrointestinal side effects as major frustrations.
Stigma cuts both ways. Some label surgery “the easy way out,” while others dismiss injections as cosmetic. Experienced clinicians remind patients that obesity is neuro-hormonal, not a character flaw; long-term success hinges on matching biology, lifestyle, and risk comfort.
When the social-media buzz fades, satisfaction tends to track results. Bigger, longer-lasting change brings the wider smiles, whether it comes from a scalpel or a syringe.
Related: